Decoding Vitrectomy: Is It Classified As A Major Surgery?
For individuals facing the prospect of a vitrectomy, apprehensions can run high. The term "surgery" itself carries weight, evoking a natural concern for the potential complexities and implications it entails. In such moments, it is vital to approach the situation with a balanced perspective. This article aims to shed light on the question that often lingers: Is a vitrectomy a major surgery? By exploring the nature of this procedure, its impact on patients, and the professional insights surrounding it, we hope to provide a clearer understanding for those wrestling with uncertainties. By the end, one may find a more nuanced perspective on this crucial aspect of eye health and the choices that lie ahead.
Is A Vitrectomy A Major Surgery?
Yes, a vitrectomy is generally considered a major surgical procedure. It involves the removal or replacement of the vitreous gel inside the eye, which is a clear, jelly-like substance that fills the space between the lens and the retina. This procedure is performed to address various eye conditions, such as retinal detachment, severe eye trauma, macular holes, and certain types of diabetic eye disease.
While vitrectomies are typically conducted by ophthalmologists who specialise in retina surgery, and the procedure itself is considered safe and routine for experienced surgeons, it is important to recognise that any surgery involving the eyes carries inherent risks. These may include infection, bleeding, changes in intraocular pressure, cataract formation, and, in rare cases, damage to surrounding structures.
Ultimately, the classification of surgery as "major" may depend on individual perspectives and experiences. For someone undergoing a vitrectomy, it is important to have a thorough discussion with their healthcare provider to understand the specific details, risks, benefits, and expected outcomes associated with the procedure. This will help them make an informed decision and alleviate any concerns they may have.
Preparing For The Treatment
Preparing for a vitrectomy involves careful planning and coordination between the clinic or healthcare facility and the individual undergoing the procedure. Here are some steps that both parties can take to ensure a smooth and successful treatment:
For The Clinic
Patient Education
Provide the individual with detailed information about the vitrectomy procedure, including what to expect before, during, and after the surgery. Address any questions or concerns they may have.
Medical History and Evaluation
Conduct a thorough pre-operative assessment of the individual's medical history, including any pre-existing conditions, allergies, medications, and previous eye surgeries. This information will help in tailoring the procedure and anaesthesia to the patient's specific needs.
Coordination with Anesthesia Team
If general anaesthesia or sedation is involved, ensure close coordination with the anaesthesia team to review the patient's medical history and discuss any specific anaesthesia considerations.
Pre-Operative Instructions
Provide the individual with clear and detailed instructions on how to prepare for the surgery. This may include fasting guidelines, medication adjustments, and any specific pre-operative care.
Informed Consent
Ensure that the individual understands the procedure and its associated risks and benefits. Obtain informed consent, and address any additional questions or concerns they may have.
Surgical Team Preparedness
Ensure that the surgical team is well-prepared, with all necessary equipment, instruments, and supplies readily available.
Sterilisation and Infection Control
Follow strict sterilisation protocols to maintain a sterile surgical environment and reduce the risk of post-operative infections.

For The Individual
Pre-Operative Consultation
Attend any pre-operative consultations with the surgeon and healthcare team to discuss the procedure, ask questions, and address any concerns.
Medical History Disclosure
Provide a complete and accurate medical history, including any allergies, current medications, and previous surgeries or eye conditions.
Follow Pre-Operative Instructions
Adhere to all pre-operative instructions provided by the clinic, which may include fasting, medication adjustments, and hygiene protocols.
Arrange Transportation
Arrange for a responsible adult to drive you to and from the clinic on the day of the surgery, as you may be temporarily unable to drive.
Plan for Recovery
Arrange for someone to stay with you during the initial recovery period, and make any necessary accommodations at home for a comfortable and safe recovery.
Post-Operative Care Instructions
Familiarise yourself with the post-operative care instructions provided by the clinic. This may include eye drops, activity restrictions, and follow-up appointments.
By ensuring effective communication and careful preparation, both the clinic and the individual can work together to optimise the outcome of the vitrectomy procedure.

Popular Questions About Vitrectomy Surgery
How painful is a vitrectomy?
During a vitrectomy, patients typically receive local anaesthesia to numb the eye and surrounding area, and some may also be given sedation or general anaesthesia for added comfort. As a result, the procedure itself is generally not painful. However, after the anaesthesia wears off, patients may experience some discomfort or mild pain, which can vary depending on factors like the complexity of the surgery, individual pain tolerance, and any pre-existing conditions.
Common post-operative sensations include soreness, a feeling of pressure or fullness, a sensation of a foreign body in the eye, light sensitivity, and mild tearing or discharge. Following post-operative care instructions, such as using prescribed eye drops and avoiding strenuous activities, is crucial for a smooth recovery. While some discomfort is normal, any severe or worsening pain should be promptly reported to the surgeon, as it could indicate a complication.
Are you awake during the surgery?
All patients receive local anaesthesia to numb the eye and surrounding area. Additionally, some patients may receive sedation or general anaesthesia to help them relax or even to induce a light sleep-like state. The choice of anaesthesia depends on various factors, including the patient's comfort level and the complexity of the surgery. The surgical team monitors the patient's vital signs throughout the procedure to ensure their safety and well-being.
Can I walk after a vitrectomy?
Yes, you can typically walk after a vitrectomy. The procedure itself does not affect your ability to walk or engage in normal activities. However, immediately after the surgery, you may experience some temporary changes in vision, such as blurriness or distortion, due to the effects of the anaesthesia and swelling in the eye. It's important to have someone available to assist you with transportation and support after the surgery, especially if you received sedation or general anaesthesia. Additionally, your surgeon will provide specific post-operative instructions regarding activities, which may include recommendations to avoid strenuous exercise or activities that could put a strain on your eyes. Always follow your surgeon's guidance for the best and safest recovery.
Do you have to sleep face down after the operation?
In some cases, particularly for specific retinal conditions like macular hole or certain types of retinal detachment, patients may be advised to maintain a face-down position after a vitrectomy. This positioning helps facilitate the healing process and allows the treated area to properly adhere and recover.
However, not all vitrectomy procedures require face-down positioning, and it's essential to follow the specific post-operative instructions provided by your surgeon. They will provide detailed guidance on any required positioning, as well as other important aspects of your recovery, such as restrictions on physical activity, use of prescribed medications, and scheduled follow-up appointments.
How long do you have to keep your head down after a vitrectomy?
The duration of face-down positioning after a vitrectomy can vary depending on the specific condition being treated and the surgeon's recommendations. In some cases, patients may be advised to maintain a face-down position for a certain number of hours per day, typically ranging from several days to a few weeks.
For instance, after a vitrectomy for a macular hole repair, patients may be instructed to maintain a face-down position for a significant portion of their waking hours, often ranging from 50 to 90 minutes per hour, for a period of one to two weeks. The exact duration and positioning requirements will be determined by your surgeon based on the specifics of your condition and the surgical approach.
How long does it take for vision to return to normal?
The timeline for vision to return to normal after a vitrectomy can vary widely depending on several factors, including the specific condition being treated, the complexity of the surgery, and individual healing patterns. In many cases, patients may experience improvements in vision within the first few days to weeks following the procedure. However, it's important to note that full visual recovery can take several weeks to several months.
For example:
- Macular Hole Repair: After a vitrectomy to repair a macular hole, significant visual improvement may be noticed within a few weeks, but complete healing and optimal visual acuity might take several months.
- Retinal Detachment: In cases of retinal detachment repair, visual recovery may be more gradual, and it may take several weeks to months for vision to stabilise.
- Other Conditions: For other conditions, such as diabetic retinopathy or vitreous hemorrhage, visual recovery can vary widely based on the specifics of the case.
How long is the surgery for a vitrectomy?
The duration of a vitrectomy surgery can vary depending on several factors, including the specific condition being treated, the complexity of the procedure, and the surgeon's experience. On average, a vitrectomy procedure typically takes between 45 minutes and 1 hour to complete. However, more complex cases or those involving additional procedures may take longer.
For example:
- Macular Hole Repair: A vitrectomy to repair a macular hole may take around 1.5 hours, depending on the size and location of the hole.
- Retinal Detachment: Repairing a retinal detachment often involves a vitrectomy, which may take approximately 2 hours or more, depending on the complexity of the detachment and the need for additional procedures like scleral buckling or gas tamponade.
- Diabetic Retinopathy: Vitrectomies for advanced diabetic eye disease can vary in duration based on the extent of the disease and any associated complications.
Can vision get worse after a vitrectomy?
Yes, in some cases, vision can temporarily worsen after a vitrectomy before it improves. This is a normal part of the healing process and is often due to factors such as inflammation, swelling, and changes in the eye's internal pressure. It's important to understand that immediate visual improvement is not always guaranteed, and patience is key.
However, if vision worsens significantly or persists for an extended period after the surgery, it's crucial to promptly consult your surgeon. This could indicate a potential complication or the need for further evaluation.
Additionally, for certain conditions that require vitrectomy, such as those involving retinal detachment or advanced diabetic eye disease, the underlying disease itself can impact visual outcomes. The success of the surgery in stabilising or improving vision depends on the specifics of the case.
Ultimately, the best way to address concerns about post-operative vision changes is to communicate openly with your surgeon. They can provide you with personalised information about what to expect during the recovery period based on your specific condition and surgical procedure.
Will I need new glasses?
After a vitrectomy, you may need new glasses, particularly if there have been significant changes in your refractive error (the need for glasses or contact lenses) as a result of the surgery.
Here are a few considerations:
- Changes in Refractive Error: The removal or alteration of the vitreous during a vitrectomy can sometimes lead to changes in the shape and position of the lens inside the eye. This may affect your refractive error, potentially necessitating an adjustment in your prescription.
- Post-operative Healing: It's important to allow for sufficient healing time before obtaining new glasses. Vision may continue to stabilise over a period of weeks to months after the surgery.
- Consult with Your Ophthalmologist: Your ophthalmologist will be able to assess your vision and advise you on whether new glasses are needed. They will conduct a thorough examination and, if necessary, perform refraction tests to determine your precise prescription.
- Temporary Changes: Keep in mind that any immediate post-operative changes in vision may be temporary. Your surgeon will provide guidance on when it's appropriate to consider obtaining new glasses.
- Potential for Long-Term Improvement: In some cases, a vitrectomy may lead to significant improvements in visual acuity, potentially reducing your reliance on glasses or contact lenses.
Are you under anesthesia?
Yes, during a vitrectomy procedure, patients typically receive anaesthesia to ensure they don't feel any pain. The type of anaesthesia used can vary:
- Local Anesthesia: This is the most common type used for all vitrectomy procedures. It involves numbing the eye and the surrounding area using anaesthetic eye drops and injectionss. With local anaesthesia, you remain conscious during the surgery.
- Sedation: In some cases, patients may also receive sedation in addition to local anaesthesia. This helps them relax and may induce a light sleep-like state. However, they can still respond to instructions from the surgical team.
- General Anesthesia: In rare cases or for specific medical reasons, a patient may receive general anaesthesia, which puts them in a deep sleep for the duration of the procedure.
The choice of anaesthesia depends on various factors, including the patient's comfort level, the complexity of the surgery, and the surgeon's preference.
What are the odds of retinal detachment?
The likelihood of experiencing a retinal detachment can vary based on a variety of factors, including age, underlying eye conditions, and previous eye surgeries.
Here are some general statistics:
- Population Risk: In the general population, the risk of developing a retinal detachment is relatively low. It's estimated to be around 1 in 10,000 people per year.
- Age: The risk of retinal detachment increases with age. It is more common in individuals over the age of 40.
- Previous History: If an individual has had a retinal detachment in one eye, they are at higher risk for a detachment in the other eye.
- High Myopia (Nearsightedness): People with high degrees of myopia (nearsightedness) have a higher risk of retinal detachment due to structural changes in the eye.
- Trauma: Severe eye trauma can increase the risk of retinal detachment.
- Family History: There may be a genetic component, so individuals with a family history of retinal detachment may have a slightly elevated risk.
- Other Eye Conditions: Certain eye conditions, such as lattice degeneration, can increase the risk of retinal detachment.
Is vitrectomy the same as cataract surgery?
No, a vitrectomy is not the same as cataract surgery. They are two distinct surgical procedures performed on different parts of the eye to address different conditions.
Vitrectomy
- A vitrectomy is a surgical procedure involving the removal or replacement of the vitreous gel inside the eye.
- It is typically performed by a retinal specialist and is used to treat conditions affecting the retina and vitreous, such as retinal detachment, macular hole, diabetic retinopathy, and vitreous hemorrhage.
- During a vitrectomy, tiny incisions are made in the eye, and specialised instruments are used to remove or manipulate the vitreous gel.
Cataract Surgery
- Cataract surgery is a procedure that involves the removal of a cloudy lens (cataract) from the eye and its replacement with an artificial intraocular lens (IOL).
- This surgery is performed by an ophthalmologist and is primarily used to treat cataracts, which are a clouding of the eye's natural lens, causing blurred vision and visual impairment.
- During cataract surgery, a small incision is made in the eye, and the cloudy lens is emulsified and removed using ultrasound or other techniques. An artificial IOL is then implanted to restore clear vision.
While both vitrectomy and cataract surgery are eye surgeries, they target different parts of the eye and serve different purposes. They may, however, be performed in conjunction with each other in certain cases where both procedures are needed to address specific eye conditions.
Will vision be completely restored?
The extent to which vision is restored after a vitrectomy depends on several factors, including the specific condition being treated, the severity of the condition, the success of the surgery, and individual healing patterns. In some cases, vision can be significantly improved, while in others, it may stabilise at a certain level.
Here are some considerations:
- Macular Hole Repair: After a successful macular hole repair, significant visual improvement is often achievable. Some individuals experience substantial restoration of central vision.
- Retinal Detachment: For retinal detachment repair, visual outcomes can vary widely. Some individuals experience significant improvement, while others may have more modest gains, depending on factors like the extent of the detachment and any pre-existing conditions.
- Diabetic Retinopathy: The impact on vision following a vitrectomy for diabetic retinopathy depends on the severity of the disease. In some cases, visual acuity can be preserved or improved.
- Individual Healing Patterns: Each person's eyes heal differently, so individual outcomes can vary.
- Pre-existing Conditions: The presence of other eye conditions or diseases can also influence visual outcomes.
Does a vitrectomy get rid of floaters?
Yes, a vitrectomy can potentially help reduce or eliminate floaters in some cases. Floaters are caused by small specks or strands in the vitreous gel that cast shadows on the retina, leading to the perception of spots or lines in your field of vision.
During a vitrectomy, the vitreous gel is removed from the eye and replaced with a clear solution. This can potentially alleviate floaters, especially if they are located in the vitreous gel itself. However, it's important to note that not all floaters can be eliminated through a vitrectomy.
Factors to consider:
- Location of Floaters: Floaters that are located in the vitreous gel are more likely to be affected by a vitrectomy. Those that are attached to the retina may not be removed.
- Risk-Benefit Assessment: The decision to undergo a vitrectomy for floaters should be carefully weighed, as any surgery carries inherent risks. It's typically considered when floaters significantly impair daily activities or quality of life.
- Other Treatment Options: Before considering surgery, your ophthalmologist may explore other treatment options, such as laser therapy (for specific types of floaters) or observation, especially if the floaters are not significantly impacting vision.
- Realistic Expectations: While a vitrectomy may reduce floaters, it's important to have realistic expectations. Complete elimination is not always possible, and there may be some residual floaters.
Ultimately, the decision to undergo a vitrectomy for floaters should be made in consultation with an experienced ophthalmologist who can assess your specific situation and provide personalised recommendations based on the location, type, and impact of the floaters.
What does vision look like with vitreous detachment?
When a vitreous detachment occurs, it can lead to various visual symptoms.
Here's what vision might be like during a vitreous detachment:
Floaters
Floaters are one of the most common symptoms of vitreous detachment. They appear as small, dark spots, specks, or cobweb-like shapes that seem to float in your field of vision. These floaters are actually shadows cast on the retina by clumps of gel or cells that have detached from the retina.
Flashes of Light
Some individuals may experience flashes of light, which can be described as brief, bright, and flickering sensations in the peripheral vision. These flashes occur when the vitreous tugs on the retina as it detaches.
Blurry or Cloudy Vision
You may notice a temporary blurriness or cloudiness in your vision, particularly in the affected eye.
Peripheral Vision Changes
Some people report changes in their peripheral (side) vision, often described as a sense of curtain-like shadows or distortions.
Sensation of a Veil or Cobweb
In some cases, individuals might describe a sensation of a veil or cobweb obstructing their vision, especially if the vitreous is not detaching smoothly.
Can dry eyes cause vitreous detachment?
Dry eyes themselves do not directly cause vitreous detachment. However, certain eye conditions or factors associated with dry eyes could potentially contribute to an increased risk of vitreous detachment. Here's how they can be related:
- Age-Related Factors: Both dry eyes and vitreous detachment are more common as individuals age. The natural ageing process can lead to changes in the consistency of the vitreous gel, making it more likely to detach.
- Inflammation and Eye Health: Chronic dry eye can lead to ocular surface inflammation and discomfort. Inflammation within the eye may potentially contribute to changes in the vitreous.
- Underlying Conditions: Conditions that are associated with both dry eyes and vitreous detachment, such as diabetes or certain autoimmune disorders, could potentially increase the risk of both conditions occurring.
- Rubbing of Eyes: Individuals with dry eyes may be more prone to rubbing their eyes, which can potentially increase the risk of retinal tears or detachment, which is a separate condition but sometimes mistaken for vitreous detachment.
While there may be some associations between dry eyes and vitreous detachment, it's important to note that vitreous detachment is a natural process that can occur in anyone, regardless of their eye health. It's primarily related to age and changes in the consistency of the vitreous gel. There is also a separate treatment process for dry eyes.
How do you stop vitreous separation?
Vitreous separation, also known as vitreous detachment, is a natural process that occurs with age and is not preventable. It happens when the vitreous gel inside the eye shrinks and pulls away from the retina. This is a normal part of the ageing process and usually does not cause any harm.
While you cannot prevent vitreous detachment, there are a few things you can do to promote overall eye health and potentially reduce the risk of related complications:
- Regular Eye Exams: Routine eye examinations by an ophthalmologist or optometrist can help detect and monitor any changes in your eye health, including the status of the vitreous.
- Avoid Eye Trauma: Protecting your eyes from injury or trauma is important. Safety measures, such as wearing protective eyewear during certain activities, can help minimise the risk of eye injuries.
- Manage Underlying Conditions: If you have conditions like diabetes or high blood pressure, keeping them well-managed with appropriate medical care and lifestyle adjustments can support overall eye health.
- Avoid Eye Rubbing: Rubbing your eyes vigorously can potentially increase the risk of retinal tears or detachments, which is a separate condition from vitreous detachment. It's advisable to avoid excessive eye rubbing.
- Seek Prompt Medical Attention: If you experience sudden and severe changes in vision, a shower of floaters, or flashes of light, seek immediate medical attention. These symptoms could indicate a more serious condition, such as a retinal tear or detachment.
Vitreous detachment is a natural and common occurrence, and in most cases, it does not require any specific intervention. If you have concerns about your eye health or any related symptoms, consult with an eye care professional for a thorough evaluation and appropriate guidance.
Can dehydration cause vitreous detachment?
Dehydration itself is not a direct cause of vitreous detachment. Vitreous detachment is primarily related to the natural ageing process and changes in the consistency of the vitreous gel inside the eye.
However, dehydration can potentially contribute to certain eye discomforts and symptoms that might be mistaken for or associated with vitreous detachment.
For example:
- Dry Eyes: Dehydration can lead to dry eyes, where the eyes do not produce enough tears to maintain proper moisture. Dry eyes can cause discomfort, irritation, and a gritty or burning sensation.
- Blurry Vision: In cases of severe dehydration, there may be some impact on vision due to changes in the tear film and the cornea's refractive properties. This can lead to temporary blurred vision.
Is vitrectomy urgent?
A vitrectomy may be considered urgent or semi-urgent in specific situations, particularly when it is needed to address serious eye conditions that could lead to vision loss or other complications if not treated promptly. Some scenarios in which a vitrectomy might be considered urgent include:
Retinal Detachment
If a patient has a retinal detachment, which is a serious condition where the retina pulls away from the back of the eye, a vitrectomy may be necessary to repair the detachment and restore vision. This is typically considered an urgent procedure.
Vitreous Hemorrhage
In cases where there is a significant bleed into the vitreous gel (vitreous hemorrhage), a vitrectomy may be required to remove the blood and address any underlying issues. The urgency depends on the extent of the bleeding and associated symptoms.
Macular Hole or Pucker
For certain macular conditions like a full-thickness macular hole or epiretinal membrane, a timely vitrectomy may be recommended to prevent further vision loss or improve visual outcomes.
Endophthalmitis
In cases of severe eye infection (endophthalmitis), a vitrectomy may be performed as part of the treatment to remove infected tissue and debris.
Traumatic Eye Injury
In cases of severe eye trauma, a vitrectomy may be urgently required to address any internal damage and restore vision.
While a vitrectomy can be an urgent procedure in these situations, it's important to note that not all vitrectomies are considered urgent. The timing of the surgery will depend on the specific condition, its severity, and the recommendations of the ophthalmologist.
What are the recovery times?
The recovery time after a vitrectomy can vary widely depending on the specific condition being treated, the complexity of the surgery, and individual healing patterns. Here are some general guidelines for recovery times after a vitrectomy:
- Immediate Postoperative Period (First Few Days):
- You may experience some discomfort, redness, and swelling in the eye immediately after the surgery.
- Vision may be blurry or hazy, and you may notice floaters. This is normal and expected.
- You may be advised to avoid strenuous activities and to keep your head in a specific position if instructed by your surgeon.
- First Week to Two Weeks:
- During this time, you will likely have follow-up appointments with your surgeon to monitor your progress.
- You may be prescribed medicated eye drops to help with healing and prevent infection.
- Some improvement in vision may be noticeable, but it may not yet be fully restored.
- First Month:
- Vision may continue to improve over the first month, but it's important to be patient as it can vary widely from person to person.
- Depending on the specific condition and surgery, you may gradually resume normal activities. Your surgeon will provide guidance on any restrictions.
- Several Months:
- It can take several months for vision to stabilise and for you to experience the full benefits of the surgery, especially for conditions like macular hole repair or retinal detachment.
- Long-Term Recovery:
- While significant improvements in vision are often achievable, it's important to have realistic expectations. In some cases, there may be residual visual changes.
It's important to strictly follow all post-operative instructions provided by your surgeon, including the use of prescribed medications, any restrictions on activities, and attending all scheduled follow-up appointments.
Keep in mind that individual recovery experiences can vary, and your surgeon will provide you with the most accurate information based on your specific condition and surgical procedure.
The chart illustrates the anticipated recovery times following vitrectomy surgery. It categorises the recovery process into distinct phases: "First Few Days," "1-2 Weeks," "First Month," "Several Months," and "Longer Recovery." Each category corresponds to the expected duration in days. For instance, the first few days post-surgery involve initial healing and adjustment, typically spanning around 3 days. The subsequent 1-2 weeks encompass a crucial phase of early recovery, lasting approximately 14 days. The first-month accounts for the primary stage of recuperation, spanning roughly 30 days. As time progresses, the recovery period extends to several months, emphasising the gradual nature of healing. Finally, an extended, longer-term recovery phase spans around 180 days, signifying the patient's journey towards full restoration of visual function and overall well-being. This chart provides a clear visual representation of the expected recovery timeline for individuals undergoing vitrectomy surgery.
Is vitrectomy worth it?
The decision to undergo a vitrectomy is highly individual and depends on various factors, including the specific eye condition being treated, its severity, and your personal circumstances. It's important to weigh the potential benefits against any associated risks or discomfort. Here are some considerations:
Potential Benefits:
- Improved Vision: A vitrectomy can often lead to significant improvements in vision, especially for conditions like macular hole, retinal detachment, or vitreous hemorrhage.
- Prevention of Further Complications: In cases of retinal detachment or other serious conditions, a vitrectomy may be necessary to prevent further vision loss or complications.
- Resolution of Symptoms: For conditions like vitreous floaters that significantly impact the quality of life, a vitrectomy may provide relief.
Considerations and Potential Drawbacks:
- Risks of Surgery: Like any surgical procedure, a vitrectomy carries risks, including infection, bleeding, retinal tears, and other potential complications.
- Recovery and Healing Time: Recovery after a vitrectomy can take time, and it's important to follow post-operative instructions carefully.
- Realistic Expectations: It's important to have realistic expectations about the potential outcomes of the surgery. Complete restoration of vision may not always be possible.
- Alternative Treatments: Depending on the specific condition, there may be alternative treatments or approaches to consider before opting for a vitrectomy.
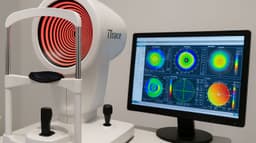
Restore Your Vision with Cutting-Edge Vitrectomy Technology at My-iClinic!
Are vision concerns affecting your daily life? Experience the latest advancements in eye care with our state-of-the-art vitrectomy procedures. Our expert team at My-iClinic is dedicated to delivering the best results possible for your vision.
4 reasons to choose My-iClinic for Vitrectomy!
- Board-certified ophthalmologists with extensive experience
- Utilising cutting-edge technology for precise and effective procedures
- Personalised care tailored to your unique eye health needs
- Comprehensive pre- and post-operative support for a smooth journey
- Located in London for easy commute and hotels to stay over.
Don't let vision issues hold you back! Take the first step towards a clearer, brighter vision. Schedule your consultation with My-iClinic today!
Find out more by Speaking to our team