Exploring The Diverse Types Of Retinal Detachment
Retinal detachment, a serious ocular condition, encompasses a spectrum of distinct manifestations, each with its own unique characteristics and underlying causes. Understanding these diverse types of retinal detachment is fundamental in tailoring effective treatment strategies for affected individuals. From the common rhegmatogenous detachment to the less frequently encountered tractional and exudative detachments, each variant demands specialised care to ensure the best possible outcomes. In this exploration, we delve into the intricacies of these different types, shedding light on the critical nuances that guide ophthalmologists towards precise and effective interventions.
What Are The Different Types Of Retinal Detachment?
Rhegmatogenous Retinal Detachment (RRD)
Rhegmatogenous Retinal Detachment (RRD) stands as the most prevalent form of retinal detachment. This condition emerges from age-related changes within the eye, particularly alterations in the vitreous gel. As individuals age, the vitreous may become more liquid and contract, potentially leading it to separate from the retina. This separation can result in a tear or hole, allowing fluid from the vitreous cavity to pass through and create a detachment.
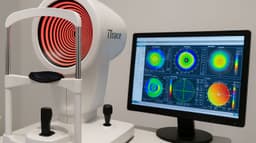
Common symptoms of RRD encompass sudden onset floaters, flashes of light, and the perception of a shadow or curtain-like movement in the visual field. Several factors can heighten the risk of RRD, including ageing, nearsightedness, previous eye trauma or surgery, and a familial predisposition. To diagnose RRD, an ophthalmologist conducts a comprehensive eye examination, often dilating the pupils for a clearer view of the retina. Additional tests like ultrasound or optical coherence tomography (OCT) may be employed to assess the extent of the detachment.
The primary approach to treating RRD involves surgical intervention. Various techniques, such as vitrectomy to remove the vitreous gel or scleral buckling to support the retina, are utilised to repair the detachment. In certain cases, a gas bubble may be introduced into the eye to aid in reattaching the retina. With prompt and appropriate treatment, the prognosis for RRD is generally favourable, often resulting in significant improvements in vision. Postoperatively, patients will require regular follow-up appointments to monitor progress and may need to observe precautions to safeguard the healing process. Early detection and intervention remain paramount for a successful outcome in cases of RRD, underscoring the critical importance of seeking immediate medical attention if a retinal detachment is suspected.
Tractional Retinal Detachment (TRD)
Tractional Retinal Detachment (TRD) represents a distinct form of retinal detachment characterised by the presence of scar tissue or fibrous membranes on the surface of the retina. These adhesions exert traction, effectively pulling the retina away from its normal position. TRD often arises as a consequence of underlying conditions, such as proliferative diabetic retinopathy or advanced stages of certain eye diseases, where abnormal growth of blood vessels and fibrous tissue occurs on the retina's surface. This condition necessitates a specialised approach in both diagnosis and treatment due to its unique underlying causes.
Symptoms of TRD may include gradual blurring of vision, visual distortion, and, in more advanced cases, the appearance of a shadow or curtain-like effect in the visual field. The risk factors for developing TRD are primarily tied to conditions that stimulate the growth of abnormal fibrous tissue on the retina. These may include uncontrolled diabetes, severe retinopathy, or inflammatory disorders of the eye. A thorough eye examination by an ophthalmologist, supplemented by imaging techniques like optical coherence tomography (OCT), is typically employed to diagnose TRD and assess its extent.
Treatment of TRD often necessitates surgical intervention to alleviate the traction exerted on the retina. Techniques may involve membrane peeling, which involves delicately removing the fibrous adhesions, or the use of endolaser to address the underlying pathology. Understanding the unique nature of TRD and its association with specific underlying conditions is pivotal in tailoring the most effective treatment strategy. Early detection and intervention are paramount in mitigating potential vision loss associated with Tractional Retinal Detachment. This underscores the importance of seeking immediate medical attention if symptoms suggestive of TRD are observed.
Exudative (or Serous) Retinal Detachment
Exudative (or Serous) Retinal Detachment, a distinctive form of retinal detachment, is characterised by the accumulation of fluid beneath the retina. Unlike other types, this detachment doesn't arise from tears or holes in the retina. Instead, it stems from underlying conditions that disrupt the normal fluid balance in the eye. Conditions such as age-related macular degeneration, central serous chorioretinopathy, or inflammatory eye diseases can lead to the leakage of fluid, resulting in a separation of the retina from the underlying layers.
Understanding this unique mechanism is crucial in devising an effective treatment approach.
Symptoms of Exudative Retinal Detachment may include a gradual onset of visual distortion, blurriness, or the perception of a shadow in the visual field. Individuals may not experience the sudden onset of floaters or flashes commonly associated with other forms of detachment. Risk factors are primarily tied to the underlying conditions causing fluid accumulation, such as age-related macular degeneration, inflammatory disorders, or certain vascular abnormalities. Diagnosis typically involves a comprehensive eye examination, supplemented by specialised imaging techniques like optical coherence tomography (OCT) to evaluate the extent of detachment.
Treatment of Exudative Retinal Detachment focuses on addressing the underlying condition causing the fluid accumulation. This may involve therapies targeting conditions like age-related macular degeneration or the use of anti-inflammatory medications for inflammatory eye diseases. Additionally, laser treatments or photodynamic therapy may be employed to seal off abnormal blood vessels and prevent further fluid leakage. Recognising the distinct nature of Exudative Retinal Detachment and its association with specific underlying conditions is pivotal in tailoring the most effective treatment strategy. Early diagnosis and intervention are crucial in managing this type of retinal detachment, underscoring the importance of seeking immediate medical attention if symptoms suggestive of Exudative Retinal Detachment are observed.

Combined Retinal Detachment
Combined Retinal Detachment is a complex form of retinal detachment that involves elements of both rhegmatogenous and tractional mechanisms. In these cases, there may be a combination of a tear or hole in the retina and the presence of scar tissue or fibrous membranes exerting traction on the retina's surface. This dual nature of detachment requires a comprehensive understanding of both underlying causes and necessitates a specialised surgical approach. Combined Retinal Detachment represents a more intricate clinical scenario, demanding a tailored treatment strategy to address the multifaceted nature of the condition.
Symptoms of Combined Retinal Detachment may encompass a range of visual disturbances, including floaters, flashes of light, and varying degrees of blurred or distorted vision. As with other types of detachment, early diagnosis is crucial for successful intervention. Risk factors may include a history of both retinal tears or holes and conditions associated with the formation of scar tissue on the retina's surface, such as proliferative diabetic retinopathy. Diagnosis involves a comprehensive eye examination, often complemented by imaging techniques like optical coherence tomography (OCT) to assess the extent and nature of the detachment.
Treatment of Combined Retinal Detachment is typically more complex due to the dual nature of the condition. Surgical approaches may involve a combination of techniques used for both rhegmatogenous and tractional detachments. This may include procedures like vitrectomy to address the tractional component and scleral buckling to support the retina in cases of a tear or hole. The nuanced understanding of the combined mechanisms underlying this type of detachment is pivotal in devising an effective and comprehensive treatment plan. Early detection and intervention are of paramount importance in cases of Combined Retinal Detachment, highlighting the critical need for prompt medical attention if symptoms suggestive of this complex form of detachment are observed.
Giant Retinal Tear
A Giant Retinal Tear (GRT) is a distinctive and relatively rare form of retinal detachment characterised by the presence of a large, full-thickness tear in the retina. These tears typically measure more than 90 degrees of the retinal circumference. Giant Retinal Tears often arise as a result of high-energy trauma or occasionally occur spontaneously. This unique nature demands a specialised approach in both diagnosis and surgical treatment due to the size and extent of the tear. Recognising the specific characteristics of a Giant Retinal Tear is pivotal in tailoring an effective surgical strategy to address this challenging form of retinal detachment.
Symptoms of a Giant Retinal Tear may include sudden onset floaters, flashes of light, and a more pronounced and rapid blurring of vision compared to smaller tears or holes. Patients may also experience a more significant visual field defect due to the size of the tear. Risk factors for developing a Giant Retinal Tear are often associated with trauma or injury, such as accidents or high-impact sports incidents. Diagnosis involves a comprehensive eye examination, supplemented by imaging techniques like ultrasound or optical coherence tomography (OCT) to evaluate the extent and characteristics of the tear.
Treatment of a Giant Retinal Tear typically requires prompt surgical intervention due to the size and potential complications associated with these tears. Techniques may involve vitrectomy to remove the vitreous gel and repair the tear, often followed by the use of a gas or silicone oil bubble to support the retina during the healing process. Recognising the unique characteristics and underlying causes of a Giant Retinal Tear is crucial in devising the most effective surgical approach. Early diagnosis and intervention are paramount in managing this type of retinal detachment, underscoring the critical importance of seeking immediate medical attention if symptoms suggestive of a Giant Retinal Tear are observed.

Congenital Retinal Detachment
Congenital Retinal Detachment is an exceptionally rare form of retinal detachment that occurs when a detachment is present at birth or shortly after. Unlike other types of detachment, which typically develop later in life due to various causes, congenital detachment is attributed to developmental abnormalities or genetic factors. This condition demands specialised care and treatment due to its unique onset in infancy or early childhood. Understanding the distinct characteristics of Congenital Retinal Detachment is essential in devising an effective approach to address this rare form of retinal detachment in paediatric patients.
Symptoms of Congenital Retinal Detachment in infants may be challenging to recognise, as they are unable to communicate visual disturbances. However, signs may include abnormal eye movements, a lack of visual response to light or objects, or the presence of a white or cloudy appearance in the affected eye. In some cases, paediatricians may detect the detachment during routine eye examinations in infancy. Congenital Retinal Detachment is a condition that is primarily attributed to genetic factors or developmental abnormalities in the eye's structure.
Treatment of Congenital Retinal Detachment typically involves surgical intervention tailored to the specific needs of the paediatric patient. The surgical approach may vary depending on the size and location of the detachment, as well as the underlying causes. It is imperative to provide early diagnosis and intervention in cases of Congenital Retinal Detachment to optimise visual outcomes and prevent further complications in paediatric patients. Recognising the unique characteristics and early onset of this condition is critical in ensuring timely and effective treatment. If any signs suggestive of Congenital Retinal Detachment are observed in infants or young children, immediate medical attention is crucial.
Each type of retinal detachment requires specific evaluation and management strategies. The choice of treatment depends on the underlying cause, the extent of detachment, and the overall health of the eye. It's crucial to consult with an experienced ophthalmologist for accurate diagnosis and appropriate treatment.
The Key Difference Between Each Detachment
| Type | Cause | Location | Symptoms | Treatment |
|---|---|---|---|---|
| Rhegmatogenous Retinal Detachment (RRD) | Tear or hole in the retina | Between neurosensory retina and retinal pigment epithelium (RPE) | Floaters, flashes of light, shadow or curtain in vision | Surgery to repair tear and reattach retina |
| Tractional Retinal Detachment (TRD) | Retinal traction due to fibrous tissue | Epiretinal surface | Gradual vision loss, distorted or wavy vision | Surgery to remove tractional forces |
| Exudative (or Serous) Retinal Detachment | Accumulation of fluid in subretinal space | Between RPE and neurosensory retina | Decreased central vision | Treat underlying cause, may include laser or injections |
| Combined Retinal Detachment | Combination of RRD and TRD | Both subretinal and epiretinal space | Various visual disturbances | Surgical intervention based on specific conditions |
| Giant Retinal Tear | Large full-thickness tear in retina | Usually starts peripherally and extends | Sudden onset of floaters, decreased vision | Emergency surgery to repair the tear |
| Congenital Retinal Detachment | Present from birth, often due to developmental issues | Variable, can involve any part of the retina | May not present symptoms immediately | Early intervention if necessary, may include surgery |
What Is The Difference Between A Retinal Tear Or Detachment?
A retinal tear and retinal detachment are related eye conditions, but they have distinct differences:
Retinal Tear
- Definition: A retinal tear occurs when the thin tissue of the retina develops a small break or rip.
- Cause: It is often caused by the shrinkage and separation of the vitreous gel from the retina, particularly as people age.
- Symptoms: Common symptoms include the sudden onset of floaters (small, dark spots or specks in your vision) and flashes of light.
- Risk Factor: Individuals who are nearsighted (myopic) or have had eye surgery or trauma may be at a higher risk.
- Severity: While a retinal tear is a serious condition, it is not as severe as a retinal detachment. However, without treatment, a tear can lead to detachment.
- Treatment: Prompt treatment, often with laser therapy or cryotherapy, can help to prevent a tear from progressing into a detachment.
Retinal Detachment
- Definition: Retinal detachment occurs when the entire retina, or a portion of it, pulls away from the underlying tissue.
- Cause: It is commonly caused by the presence of a retinal tear, which allows fluid to pass through and separate the retina from its normal position.
- Symptoms: Symptoms may include sudden onset of floaters, flashes of light, a shadow or curtain-like effect in the visual field, and a rapid blurring of vision.
- Severity: Retinal detachment is a more severe condition compared to a tear, as it involves a significant portion of the retina becoming detached.
- Treatment: Surgical intervention is typically required to reattach the retina. Different surgical techniques, such as vitrectomy or scleral buckle, may be employed based on the specific case.
In summary, a retinal tear is a small break or rip in the retina, whereas a retinal detachment is a more serious condition where the entire or a portion of the retina becomes detached from its normal position. Both conditions require prompt medical attention to prevent further vision loss. If you suspect you have a retinal tear or detachment, seek immediate care from an eye care professional.
Put Your Eyes In The Care Of Experts
Trust in My-Clinic's expert care for a comprehensive range of retinal detachment solutions. Our skilled team of ophthalmologists is dedicated to restoring your vision with precision and compassion. From Rhegmatogenous to Exudative, our specialised treatments are tailored to your unique needs. Don't compromise on your sight—schedule your consultation with My-Clinic today and experience the difference expertise makes.
Find out more by Speaking to our team