Understanding Glaucoma: What You Need To Know
Glaucoma is a condition where the pressure inside the eye becomes too high. If left untreated, this high pressure damages the optic nerve, which carries visual information to the brain. This damage is irreversible and, if severe, can lead to blindness. Treatment focuses on lowering eye pressure to prevent further vision loss.
Download Our FREE Brochure Here
In a normal eye, a fluid called aqueous humor is produced in a specialized area at the back of the iris (the coloured part of the eye). The fluid flows forward through the pupil. It is a clear, watery substance that carries nutrients to the tissues at the front of the eye. Once it has fulfilled this role, it drains through a small canal located in the angle at the front of the eye and returns to the bloodstream. The balance between fluid production and drainage maintains a stable pressure within the eye.
There are two main types of glaucoma:

Rarer Types Of Glaucoma
Other, rarer types of glaucoma include pigmentary glaucoma, pseudoexfoliation, uveitic glaucoma, traumatic glaucoma, and congenital glaucoma.
In open-angle glaucoma, the outflow blockage occurs gradually, causing pressure to rise painlessly. In angle-closure glaucoma, however, the rise in pressure tends to be sudden and very painful. In most patients with narrow angles, optometrists can detect this condition before a catastrophic angle closure occurs, and the patient is then referred for laser eye treatment.
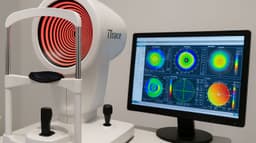
X-ray Scan Of The Human Eye

Glaucoma Risk Factors
Several factors can increase the risk of developing glaucoma, including:
- Age over 60 years old
- African descent
- Family history of glaucoma
- Reduced corneal thickness
- Severe nearsightedness (myopia) or farsightedness (hyperopia)
- Prolonged use of steroid eye drops
Tests For Glaucoma
Eye Pressure (Intraocular Pressure, IOP)
To measure intraocular pressure (IOP), a small probe is gently placed on the cornea to assess the eye’s firmness. This measurement is calibrated by assessing the thickness of the cornea for each eye. The frequency of IOP tests depends on the disease’s severity, rate of progression, and the patient's response to treatment.
Phasing
Eye pressure can fluctuate hourly, daily, or weekly. If your eye pressure readings are borderline or if glaucoma damage is progressing despite normal pressure levels observed during clinic checks, a full day of pressure measurements may be needed. This comprehensive data helps your doctor decide on the best course of action, whether it be adjusting treatment or conducting further investigations.
Optical Coherence Tomography (OCT)
This scan involves focusing on a blue dot while a laser beam scans the eye. OCT detects early changes in the thickness of the retina and nerve fibres that transmit vision to the optic nerve. By identifying these changes before vision is affected, OCT enables much earlier diagnosis and treatment of glaucoma.

Corneal Thickness Measurement
Corneal thickness is measured using laser or ultrasound. Thin corneas can cause IOP to be underestimated, while thicker corneas may lead to an overestimation. Knowing corneal thickness allows for more accurate eye pressure assessments.
Gonioscopy
A handheld contact lens with built-in mirrors is used to examine the angle where the iris meets the cornea, helping to determine if the angle is open or at risk of closing.
Visual Field Test
This test uses a machine that displays sequential white light spots of various sizes and brightness levels on a bowl-shaped screen. The patient presses a button each time they see a light spot, allowing the machine to map the brightness levels at which the patient can detect light. This test helps identify areas of vision most vulnerable to glaucoma damage.
The earliest signs of damage usually appear as areas where light needs to be brighter before being seen, often appearing above and below the line of sight. If untreated, these areas expand and merge, eventually leaving only central vision, which can also be lost in advanced stages, leading to complete blindness. Visual field tests are typically conducted every six to twelve months.
Treatment Options
Treating glaucoma effectively requires a comprehensive approach that combines the latest in diagnostic technology with the most advanced treatment methods. Best practices in glaucoma management begin with early detection using state-of-the-art equipment, such as optical coherence tomography (OCT) and visual field testing, to monitor the health of the optic nerve and assess any damage. Once diagnosed, treatment often involves medication, laser therapy, or surgical interventions, depending on the severity. Laser treatments like selective laser trabeculoplasty (SLT) are increasingly popular, offering a minimally invasive option to lower intraocular pressure. In more advanced cases, surgical options like minimally invasive glaucoma surgery (MIGS) can be used to improve drainage. Using the latest technology ensures precision and enhances the success of outcomes, helping preserve vision and improve quality of life for patients.
Your Next Step
If you're experiencing symptoms of glaucoma or are concerned about your eye health, don't wait—early detection is key to preserving your vision. At My-iClinic, we use state-of-the-art equipment to accurately diagnose and treat glaucoma with the most advanced methods available. Our expert team is here to provide personalized care and guide you through the best treatment options. Schedule a consultation with us today and take the first step toward safeguarding your eyesight for the future. Contact My-iClinic now to book your appointment!
Find out more by Speaking to our team